Any injury involving the soft tissue and /or bone of the face and skull is known as craniofacial trauma. These injuries are as diverse in their causes as they are in their severity. Craniofacial reconstruction following trauma is different for each individual as it highly depends on the nature and location of the patient’s injuries. The first priority in any trauma patients is treating problems with airway, breathing, circulation or any other life-threatening emergencies before treating facial injuries. Over 60% of patients with severe facial trauma have other serious injuries in the head, chest, or abdomen. This high rate of additional injuries reflects the enormous forces needed to fracture human facial bones. In particular, a surgeon who is examining a patient with severe facial trauma will be particularly concerned about damage to the brain, the spinal cord in the neck, and the eyes. Of note, severe facial trauma often leads to blockage of the airway thus it is important to have a protected airway before continuing trauma resuscitation and treatment of facial injuries. The second priority in treating traumatic facial injuries is controlling severe bleeding.
Common bony injuries to the face following facial trauma:
- Zygoma
- Maxilla
- Nasoethmoid Orbital Skeleton
- Orbit
- Mandible
- Soft Tissue Deformities
The location of the zygoma makes it prone to injuries despite its sturdiness. The zygomatic bone occupies a prominent and important position in the facial skeleton. It plays a key role in determining facial width as well as acting as a major support of the midface. The mechanism of injury usually involves a blow to the side of the face from a fist, object, or motor vehicle accidents. Moderate force may result in minimally or nondisplaced fractures. More severe blows result in displacement of the zygoma.


Historically, zygomatic fractures were fixed by popping the fragments back into alignment (closed reduction). Not only were these results frequently unsatisfactory, but they were also fraught with complications including visual problems, non healing of the fracture, and significant residual deformities. The treatment of zygomatic fractures has dramatically progressed over the past several decades to the more aggressive open repair (open reduction) using rigid mini-plates of titanium to stabilize a fracture and align the bones in their appropriate position. The floor of the orbit (eye socket) is routinely explored and reconstructed, if needed.
The maxilla is the largest part of the middle third of the facial skeleton. Fractures of the maxilla occur less frequently than those of the mandible or because of the strong structural support of this bone. The midface consists of alternating thick and thin sections of bone that are capable of resisting high amounts of force. This structurally strong bone provides protection for the eye socket and brain, projection of the midface, and support for the upper bite.
Maxillary fractures today are often the result of motor vehicle accidents. These high-velocity injuries are diagnosed by computerized tomographic (CT) scans. Once again, the more recent development of 3-D reconstructions have aided greatly in the diagnosis, classification, and preoperative planning of these complex maxillary fractures.
Maxillary fractures are treated by open reduction to realignment and immobilization of the bones that make up the maxilla. Establishment of pre-injury bite and midface alignment provides the foundation for this treatment. Early placement of the patient in Internal Maxillary Fixation (IMF) will decrease the chance of internal soft tissue deformities, reduce pain and restore the dental occlusion. IMF is established by securing wire arch bars to the upper and lower set of teeth. The appropriate occlusion of the teeth (or bite) is then determined and the maxillary and mandibular (jaw bone) arch bars are secured together. This is one of the simplest and most effective forms of treatment.
Recent advances in the treatment of maxillary fractures include the use of open-repair and realignment (open reduction) techniques using rigid plate and screw fixation of the facial bones. Bone grafts have been used to replace missing or severely fractured bones. This more aggressive surgical approach has dramatically improved the aesthetic results now obtainable with fewer secondary deformities.
Trauma to the central midface frequently results in fractures of the nasoethmoid orbital (NOE) skeleton. This complex area consists of a union of bones from the nose, orbits, maxilla, and cranium. These fractures may be the most difficult and challenging of all facial fractures to diagnose and treat. To the inexperienced examiner, NOE fractures may be misdiagnosed as simple nasal fractures, and a high degree of suspicion is necessary to make the diagnosis. These fractures may occur as isolated injuries or as part of more complex (Le Fort) facial fractures. Failure to diagnose these injuries or inadequate treatment will result in both functional and cosmetic deformities that are very difficult to correct secondarily.
The best results of the NOE fracture are obtained with early diagnosis and aggressive surgical treatment. Complications result when this injury has been misdiagnosed or inadequately treated. Successful surgical treatment of these complex injuries consists of early open reduction and stabilization of bone fragments. Bone grafts are used to restore contour and support to areas of severely fractured or missing bone. Unstable or displaced fractures that are left untreated result in permanent deformities once healed. Late reconstruction is a difficult task that requires repositioning of both bone and soft tissue. Although late reconstruction of these deformities is possible, in general, the best aesthetic results are obtained with definitive repair at the time of injury, avoiding the common pitfalls.
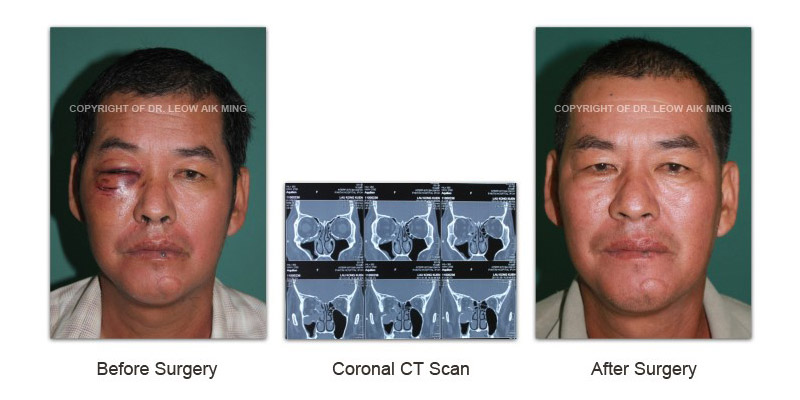
An orbital blow-out fracture consists of a fracture of the bones of the eye “socket”. This may involve the orbital floor, walls, or roof. Most cases, however, involve the orbital floor. An orbital blow-out fracture is almost always secondary to a blunt blow from a relatively large object, such as a fist, elbow, baseball bat, or severe motor vehicle accident. Most patients will present with pain, tenderness around the eye, swelling, and double vision. Despite this potential for wide variation of internal orbital fractures, there are basic principles that can be applied to aid in diagnosis and treatment. The bony orbits play a vital role in maintaining normal function and aesthetics of the eyes therefore, realignment and reconstruction of the bony orbit of the eye is essential to maintain normal function and appearance of the eyes.
A number of advances have been made in the past 10 to 15 years in the diagnosis and treatment of internal orbital fractures. These advanced techniques have allowed better exposure of the fractures and precise reduction and stabilization of the fractures. The use of mini- or microplates and metal meshes in combination with bone grafts has also improved stabilization and enhanced the healing of orbital fractures.

Because most of the bone of the internal orbit is thin and weak, it is frequently difficult to reduce and adequately stabilize without the use of autogenous or alloplastic materials. Autogenous bone grafts have been the material most often used by craniomaxillofacial/ plastic surgeons for reconstruction of the internal orbit. Split skull bone has gained popularity because of its low rate of infection and decreased resorption. Other autogenous materials that have been used include bone from the hip (iliac crest) and ribs or from cartilage. A variety of alloplastic material such as silicone, teflon, tantalum mesh, polyethylene, and methyl methacrylate have been used for orbital reconstruction. The primary concern with the use of these materials is the risk of infection.
The mandible is a unique bone having a complex role in both aesthetics of the face and functional occlusion (bite). Because of the prominent position of the lower jaw, mandible fractures are the most common fracture of the facial skeleton. Fractures of the mandible will typically reveal a malocclusion (inability to bite down), pain at fracture site, significant internal bruising, or laceration with bleeding between teeth at the fracture site.
Reduction and stabilization of the mandible fracture is the key to successful treatment. The method of management may vary based on the severity, location of the fracture and presence or absence of teeth. Mandible fractures are usually treated by closed reduction with wiring of the teeth or open reduction with internal rigid fixation using plates. Non-operative management of a mandible fracture with a soft diet is rarely indicated. The technique of closed reduction involves wiring the teeth for 4 to 6 weeks. Internal rigid fixation when performing open reduction requires exposure of the fracture sites and stabilization with plates and/or screws. Accurate reduction with good stabilization can frequently avoid complications and help to restore the patient’s primary occlusion and facial appearance.
Soft tissue deformities may involve the skin, subcutaneous tissue, underlying muscle or a combination of any of these elements. Traumatic facial injuries may be blunt, penetrating and/or avulsive in nature. An avulsion, or loss of soft tissue, may create a significant deformity which requires reconstruction. Generally the facial bony deformities are reconstructed first followed by correction of soft tissue problems.


One example of a severely deforming and psychologically crippling injury is the scalp avulsion. This presents a very challenging problem particularly if the avulsed portion is very large and cannot be replanted by microvascular technique. A new and innovative approach to this type of problem has been the use of the tissue expander. These expanders are much like deflated balloons placed beneath adjacent normal tissue. Over a period of weeks these expanders are gradually inflated, stretching the normal skin for use in reconstruction. An example of this technique is shown for reconstruction of the scalp.
PRE-OPERATIVE EVALUATION
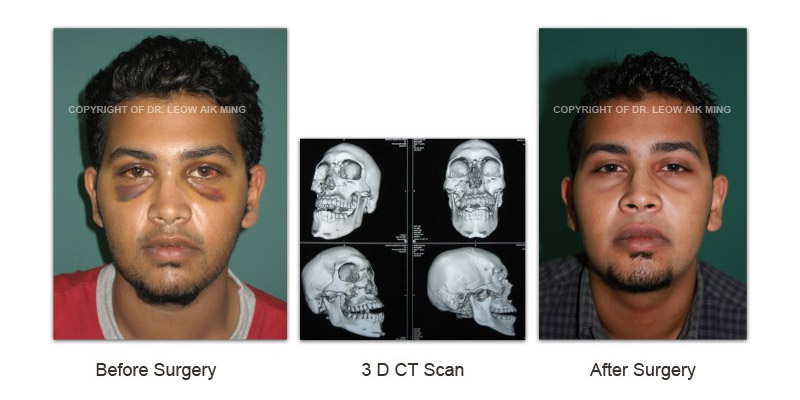
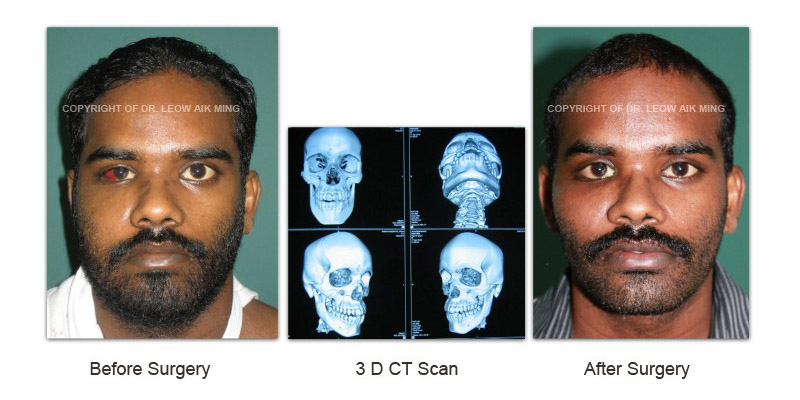
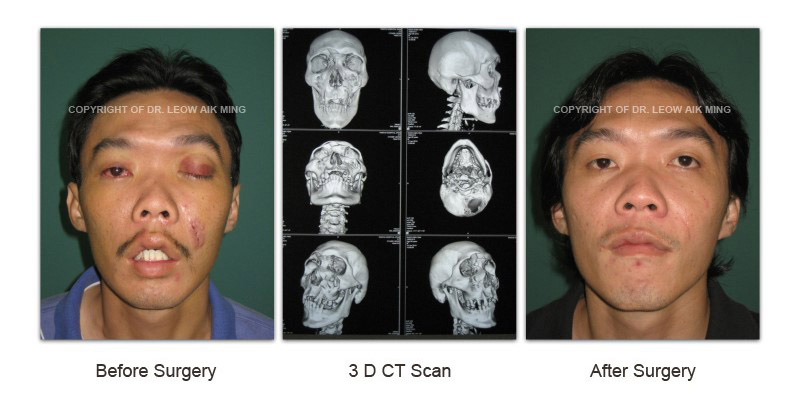
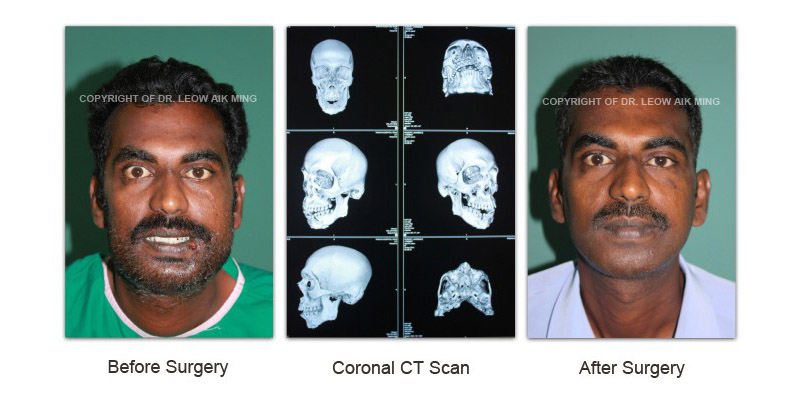
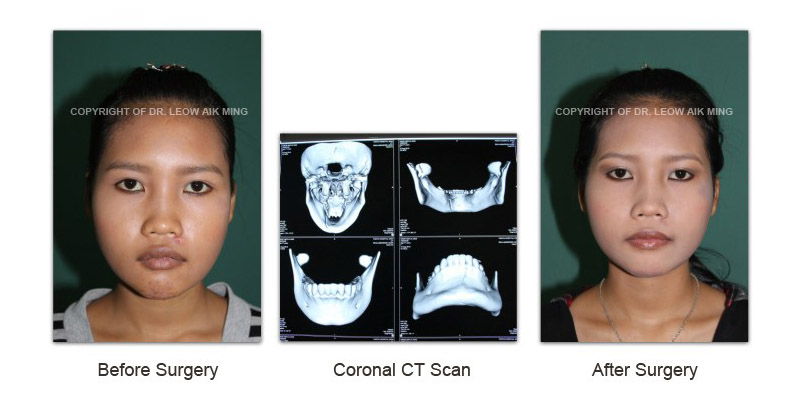
Radiological assessment of the extent of craniofacial injury is essential prior to any surgical intervention. Sometimes the radiological assessment of craniofacial injuries may need to be postponed for 24-72 hours in order to treat injuries to other organ systems. When the patient is out of immediate danger, x-ray studies and computed tomography (CT) scans are taken of the craniofacial injuries. The accurate diagnosis of facial fractures has been greatly improved by the addition of two- and three-dimensional CT scans which have replaced the plain x-rays for the diagnosis of many types of fractures. Three-dimensional reconstructions have enhanced preoperative bone analysis and planning for reconstructive surgery by providing a life-like simulation of the fractures.
Apart from these investigations mentioned prior to craniofacial trauma reconstruction, communication with the patient is vital in order to achieve the patient’s goals. During the initial consultation, patients will have the opportunity to understand their conditions and desirable outcome with the plastic surgeon. The plastic surgeon will work closely with the patients to reach an agreement about the expectations from the surgical procedures involved and their long term benefits. Every patient is different, therefore a specific treatment regimen is planned to suit an individual’s need.
PREPARATION
- Get laboratory and radiological tests or medical evaluation
- If any other associated injuries or medical conditions are present, special referral to the respective surgical or medical specialties will be done
- Evaluation of general health status and any pre-existing health conditions or risk factors
- Adjust medications if for certain medical conditions
- Special instructions will be given on the day before and after surgery
TREATMENT
The best way to prevent post-traumatic facial deformities is to obtain the appropriate treatment at the time of the injury. Delayed treatment has been replaced by early or immediate surgical treatment and stabilization of small bone fragments augmented by bone grafts and mini-plate fixation. These new advances have allowed surgeons to approach and often reach the goal of restoring pre-injury facial appearance and function in a one-stage operative repair. However, despite many surgical advances, there are still patients that end up with significant deformities. These are patients that for whatever reason are treated inadequately or because of other life-threatening injuries, cannot receive treatment of their facial injuries.
COMPLICATIONS AND RISKS
Every surgical procedure has its own complications and risks. However, if a patient is assessed properly before the surgery and postoperative care is given adequately, these risks can be eliminated or reduced. Some of the risks of craniofacial trauma reconstruction are common to all surgical procedures done under general anaesthesia. These include bleeding, breathing problems, bruises underneath the skin, reactions to the anaesthesia, and infection.
Risks that are specific to craniofacial trauma reconstruction include:
- Neurologic deficits, including motor and sensory (anaesthesia, paraesthesia) deficits
- Decrease in facial height
- Increase in facial width
- Decrease in facial projection
- Traumatic telecanthus or enophthalmos
- Malocclusion
- Nasal obstruction and deformities
- Cerebrospinal fluid leak
- Anosmia
- Blindness
Risk factors that can affect the results of craniofacial reconstruction include:
- Poor nutrition
- HIV infection
- Poor immune system
- Skin damage from radiation therapy
- Connective tissue disease, such as lupus or scleroderma
- Smoking
- Time elapsed between a traumatic injury and surgical treatment (delayed treatment)
- Poor blood circulation in the affected area
POST-OPERATIVE RECOVERY AND EXPECTATIONS
Postoperative recovery following craniofacial trauma reconstruction vary depending upon patient’s age, the extent of craniofacial injuries and other associated injuries, simple or complex surgical procedures performed and other associated surgical or medical conditions. The recovery period for craniofacial trauma reconstruction may range from weeks to months. In some cases, second surgery or revision surgery may be needed to correct any residual craniofacial deformities at later stage.
– COPYRIGHT OF DR LEOW AIK MING
